About Us
Researchers + Clinicians
Parents
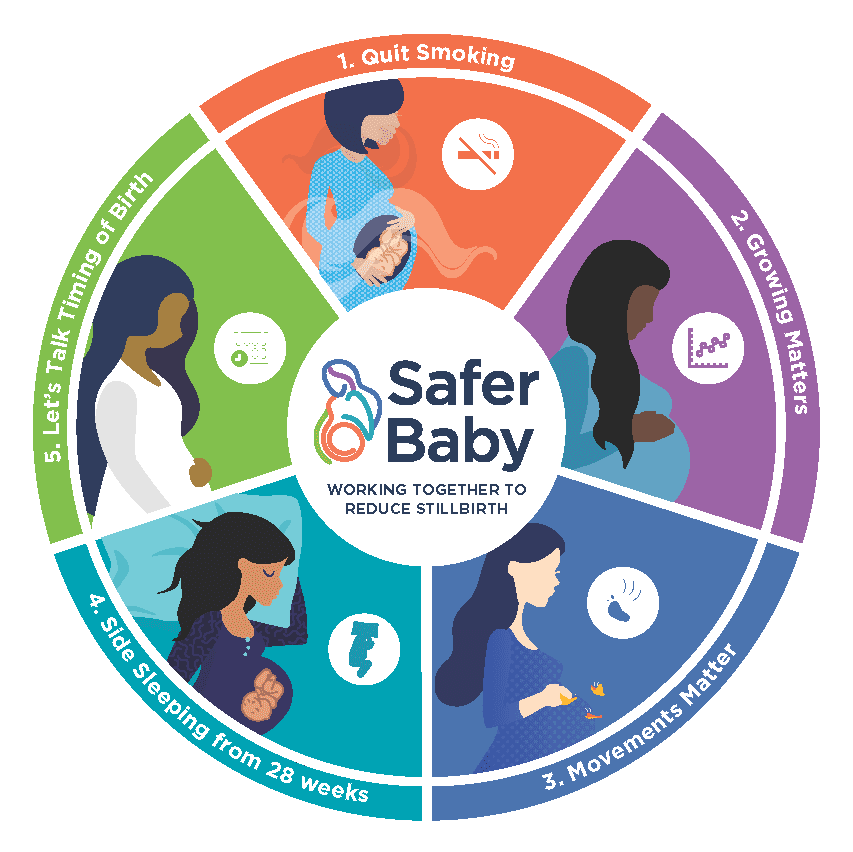
The Safer Baby Bundle is a national initiative with five evidence-based elements to address key areas where improved practice can reduce the number of stillborn babies.
The Safer Baby initiative aims to help women understand the things they can do to reduce their risk of stillbirth.
Visit our Safer Baby website for evidence-based advice for having a safer pregnancy, and explore trusted pregnancy resources to reduce the risk of stillbirth.
We are committed to reducing the inequity in Australia’s stillbirth rates. At the 2023 National Stillbirth Forum the new culturally adapted pregnancy resources were launched for First Nations women, as well as migrant and refugee women from some communities who are also disproportionately impacted by stillbirth.
This important work has involved over two years of consultation and development, and is an extension of the Safer Baby Bundle. Thank you to our partners and the organisations and individuals who contributed to the consultations and co-design of these fantastic resources. We encourage you to share them with your communities.

For First Nations women and their families to reduce the risk of Sorry Business Babies (stillbirth), the new Stronger Bubba Born resources include flyers and videos that are available at the Stronger Bubba Born website.
These resources were developed by the Stillbirth CRE Indigenous research team with the guidance of the Indigenous Advisory Group. Delivery partner Curtin University supported the extensive consultation and co-design process. The National Aboriginal Community Controlled Health Organisation (NACCHO) and the Waminda South Coast Women’s Health and Wellbeing Aboriginal Corporation are also collaborators with the CRE on their Indigenous work.

To support migrant and refugee women who experience the highest rates of stillbirth, tailored resources are now available for Arabic, Dari, Dinka, and Karen-speaking communities. These include a written booklet, summary video, and self-paced digital booklet with audio.
These resources are available at the Growing a Healthy Baby website. A network of community groups and health educators from the Multicultural Centre for Women’s Health (MCWH) and the Stronger Futures CRE at the Murdoch Children’s Research Institute (MCRI) worked with the Stillbirth CRE to develop these in-language resources.
In addition, this latest information has also been translated into 25 languages and is available on the CRE’s Safer Baby website, saferbaby.org.au/, and available with all resources for healthcare professionals at learn.stillbirthcre.org.au/.
The Stillbirth CRE has led the development of a bundle of care to address the priority evidence practice gaps in stillbirth prevention for implementation across maternity services. This work is being done in partnership with health departments across Australia and key stillbirth advocacy organisation Stillbirth Foundation Australia.
By implementing the Safer Baby Bundle elements of care, the overall goal is to reduce stillbirth in Australia by 20% for women from 28 weeks’ gestation and beyond.
In 2019, a Safer Baby Bundle Handbook and Resource Guide was created as an informational support to assist maternity healthcare professionals to implement the Bundle to their everyday practice. Free and accredited CPD training for healthcare professionals is available from our Safer Baby Bundle e-learning modules.
The Safer Baby Bundle evidence-based eLearning module provides a suite of educational resources based on the latest clinical best practice in stillbirth prevention. This eLearning package provides evidence-based and collaboratively designed learning resources for healthcare professionals working with pregnant women.
All practitioners providing maternity care are encouraged to undertake the Safer Baby Bundle eLearning module to support the provision of best practice care.
Join the team that’s reducing stillbirth in Australia. Start today!
Become a Safer Baby Bundle champion in your workplace. The Safer Baby Bundle Masterclass is an interactive presentation that has been developed for maternity health professionals as an overview of the Safer Baby Bundle eLearning.
This 60-minute Masterclass summarises the five bundle elements, highlights key evidence and clinical recommendations related to the Safer Baby Bundle, and discusses basic principles for implementation. Request a copy of the Masterclass and presenter notes today to become a Safer Baby Bundle champion in your workplace.
You can also view a PDF version below to preview the presentation and understand how you might use the Masterclass to educate colleagues about the Safer Baby Bundle.
The Safer Baby Bundle for Australian maternity healthcare professionals is a collection of change ideas or interventions for Australian maternity healthcare professionals designed to reduce late gestation stillbirth. The interventions are based on evidence summaries developed in partnership with the Perinatal Society of Australia and New Zealand (PSANZ). Development of the SBB has drawn from the expertise and experience of international advisors from the UK Saving Babies Lives Bundle of care.
A 20% reduction in stillbirth rates has been seen in the UK and Scotland, where a similar care bundle has been implemented. We believe that implementation of the Safer Baby Bundle in Australia will result in at least the same reduction in stillbirth. We think the bundle will also reduce serious adverse outcomes in live-born babies, improve health outcomes among mothers, increase mothers’ satisfaction with care, and be cost-effective.
The Safer Baby Bundle was initially developed in Australia with the health departments in New South Wales, Victoria, and Queensland, as well as key stillbirth advocacy groups Stillbirth Foundation and Still Aware. Our partnerships with Safer Care Victoria, Clinical Excellence Queensland and New South Wales Clinical Excellence Commission led to the roll-out of the Safer Baby Bundle across Australia, which is already showing promising results with a 21% reduction in stillbirth rates across participating maternity services in Victoria in 2020-21. Today, the Safer Baby Bundle has been introduced across all Australian health jurisdictions, and endorsed by a large number of advocacy groups and professional colleges. See our partners for details.
We are committed to reducing the inequity in Australia’s stillbirth rates and are working with the Department of Health and Aged Care and our partners to reach First Nations women with our Stronger Bubba Born resources, and migrant and refugee communities, with our Growing a Healthy Baby resources (co-designed for Arabic, Dari, Dinka and Karen speaking communities). These culturally adapted resources were developed over two years of consultation, co-design and tailored translations and designs.
The Stillbirth CRE has also recently translated the updated Safer Baby Bundle information into 25 languages, available on the, saferbaby.org.au/, and available with all resources for healthcare professionals at learn.stillbirthcre.org.au/.
We have established partnerships across Australia with Indigenous communities in the Northern Territory, South Australia, Queensland, and Western Australia, and are working with our Advisory Groups to create Aboriginal and Torres Strait Islander, and rural and remote versions of the Safer Baby Bundle Masterclass and resources. These resources are expected to be released later this year.
Bereaved parents discussing the importance of the Safer Baby Bundle.


Level 3, Aubigny Place
Mater Research Institute
Raymond Terrace,
South Brisbane QLD 4101
The University of Queensland Faculty of Medicine